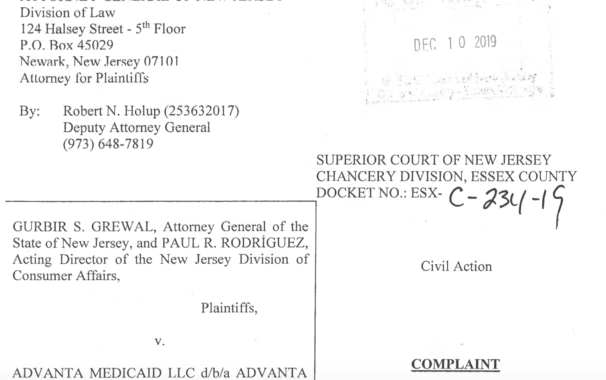
A company that was supposed to help consumers complete Medicaid applications for a fee stole more than $300,000 from clients, according to a lawsuit filed by the New Jersey attorney general and the state Division of Consumer Affairs. The State’s complaint, alleging violations of the Consumer Fraud Act, was filed in New Jersey Superior Court in Essex County.
Advanta Medicaid LLC d/b/a Advanta Medicaid Specialists (“Advanta”), which had offices in Ocean County and Waterbury, Connecticut, allegedly charged dozens of New Jersey consumers fees of between $3,000 and $9,000 to assist them in filing Medicaid applications to establish eligibility for benefits. The company offered a money-back guarantee for those not approved for Medicaid “but failed to deliver the services promised or provide full refunds as guaranteed,” the state said.
Ultimately, Advanta ceased operations abruptly, leaving consumers who had already paid for the company’s services with nowhere to turn.
The lawsuit also names as defendants two men involved with the company, Nissim “Sam” Aryeh and Chaim E. Feller, both of Ocean County. According to the complaint, Aryeh and Feller transferred company funds into their personal accounts and used those company funds to cover expenses at an Atlantic City casino — Harrah’s Resort — costs at high-end restaurants, clothing stores, bicycle rentals, car payments, furniture and flooring purchases and payments to local private schools and synagogues, the complaint said.
The Division opened its investigation after receiving dozens of complaints about Advanta. To date, more than 49 consumers or their family members who contracted with Advanta between 2014 and 2018 have reported paying upfront fees but then never receiving the services that Advanta promised or the refund it guaranteed customers who were not approved for Medicaid coverage. The suit said the state expects there are many more victims who have not yet been identified.
The State alleges the defendants violated the New Jersey Consumer Fraud Act and advertising regulations by engaging in conduct that included:
- Failing to submit applications for Medicaid services for consumers, despite the consumers paying up front in full for these services.
- Representing to consumers that Medicaid applications had been submitted when, in fact, they had not.
- Representing to consumers that the company would return their sensitive personal and financial documentation, but then failing to do so.
- Failing to honor the money-back guarantee advertised on the company’s website.
In addition to seeking restitution for injured consumers, the State’s filing seeks to impose monetary penalties for the defendants’ alleged unfair and deceptive business practices, to terminate Advanta’s business registration, to recover attorneys’ fees and investigative costs, to bar any ongoing or future unfair and deceptive business practices by the defendants, and to restrict Aryeh and Feller’s business activities in the State.
“Families and individuals seeking assistance with Medicaid enrollment are among those who can least afford to lose thousands of dollars to fraud,” New Jersey Attorney General Gurbir Grewal said in a press release. “Today we’re sending a clear message that there will be serious consequences for companies and individuals who prey on New Jersey consumers, and particularly on those who are most vulnerable.”
Consumer Affairs asks that any families who have had experiences with Advanta contact its offices. You can file online complaint or call (800) 242-5846 (toll-free within New Jersey) or (973) 504-6200.
The Consumer Fraud Complaint filed by New Jersey is attached here –
For additional information concerning Medicaid applications and appeals, visit:
Categories
- Affordable Care Act
- Alzheimer's Disease
- Arbitration
- Attorney Ethics
- Attorneys Fees
- Beneficiary Designations
- Blog Roundup and Highlights
- Blogs and Blogging
- Care Facilities
- Caregivers
- Cemetery
- Collaborative Family Law
- Conservatorships
- Consumer Fraud
- Contempt
- Contracts
- Defamation
- Developmental Disabilities
- Discovery
- Discrimination Laws
- Doctrine of Probable Intent
- Domestic Violence
- Elder Abuse
- Elder Law
- Elective Share
- End-of-Life Decisions
- Estate Administration
- Estate Litigation
- Estate Planning
- Events
- Family Law
- Fiduciary
- Financial Exploitation of the Elderly
- Funeral
- Future of the Legal Profession
- Geriatric Care Managers
- Governmental or Public Benefit Programs
- Guardianship
- Health Issues
- Housing for the Elderly and Disabled
- In Remembrance
- Insolvent Estates
- Institutional Liens
- Insurance
- Interesting New Cases
- Intestacy
- Law Firm News
- Law Firm Videos
- Law Practice Management / Development
- Lawyers and Lawyering
- Legal Capacity or Competancy
- Legal Malpractice
- Legal Rights of the Disabled
- Liens
- Litigation
- Mediation
- Medicaid Appeals
- Medicaid Applications
- Medicaid Planning
- Annuities
- Care Contracts
- Divorce
- Estate Recovery
- Family Part Non-Dissolution Support Orders
- Gifts
- Life Estates
- Loan repayments
- MMMNA
- Promissory Notes
- Qualified Income Trusts
- Spousal Refusal
- Transfers For Reasons Other Than To Qualify For Medicaid
- Transfers to "Caregiver" Child(ren)
- Transfers to Disabled Adult Children
- Trusts
- Undue Hardship Provision
- Multiple-Party Deposit Account Act
- New Cases
- New Laws
- News Briefs
- Newsletters
- Non-Probate Assets
- Nursing Facility Litigation
- Personal Achievements and Awards
- Personal Injury Lawsuits
- Probate
- Punitive Damages
- Reconsideration
- Retirement Benefits
- Reverse Mortgages
- Section 8 Housing
- Settlement of Litigation
- Social Media
- Special Education
- Special Needs Planning
- Surrogate Decision-Making
- Taxation
- Technology
- Texting
- Top Ten
- Trials
- Trustees
- Uncategorized
- Veterans Benefits
- Web Sites and the Internet
- Webinar
- Writing Intended To Be A Will







Vanarelli & Li, LLC on Social Media